Books |
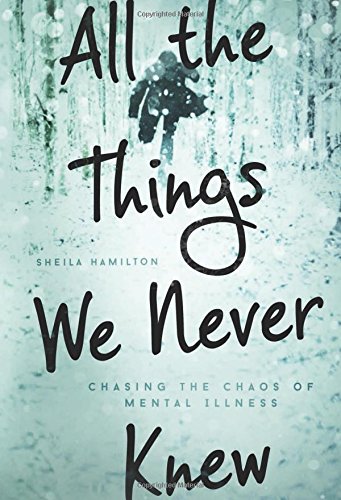
All the Things We Never Knew: Chasing the Chaos of Mental Illness
Sheila Hamilton
By
Published: Oct 14, 2015
Category:
Health and Fitness
Sheila Hamilton’s business is getting the story. She does it very well — as a television reporter, she’s won five Emmys. In Portland, Oregon, where she hosts the morning drive-time show on KINK FM, she uses her celebrity to promote good causes and creative people.
But there is a story she missed, and it’s huge — the suicide of her husband. She tells that story, and much more, in “All the Things We Never Knew: Chasing the Chaos of Mental Illness.” Here’s how the book starts:
I missed much of the unfolding of my husband’s mental illness. By the time I pieced together the puzzle of who David actually was, he was falling apart. My once brilliant, intense and passionate partner was dead within six weeks of a formal diagnosis of bipolar disorder, leaving my nine-year-old daughter and me without so much as a note to understand his decision. He’d left us hundreds of thousands of dollars in debt, and with no plan for helping us recover from the profound grief of his suicide.
Well, you knew a story like this would be a nightmare. Still, the day-by-day account is an irresistible page-turner. David paying no attention to his business, losing weight until he’s skeletal, destroying every shred of his wife’s love. David repentant, swearing he’d make things right. David cutting his wrists, charming his way out of the hospital. David, breaking into a home, stealing a gun. David in the snow, his legs crossed, a hole in his head, looking finally at peace. His daughter as her mother tells her the news, making the sound of “the crippling of her heart.”
But that fast-motion train wreck, exquisitely told, is only half the book. The other half is a well-reported mental health guide that could be a primer for anyone who’s aware that something is wrong with a friend, loved one or him/herself but doesn’t know what to do. Taken together, Hamilton’s book is both powerful and useful: a picture of the man who died and the woman who survived him, and her commitment to help others from acquiring her expensive education. [To buy the book from Amazon, click here. For the Kindle edition, click here. For the audio book, recorded by the author, click here.]
I can attest to Sheila Hamilton’s skill as an interviewer; when we talked, there was no place to hide. Just before her book was published, I grilled her.
Jesse Kornbluth: 57% of people with bipolar disorder say they have trouble controlling the urge to have sex with someone other than their partner. Patients with depressive and manic depressive illness are more likely to commit suicide than patients in any other medical or psychiatric risk group — their mortality rate is higher than it is for most types of heart disease and cancer. More people die of suicide than car accidents. Given that, why do doctors downplay the dangers of these mental illnesses?
Sheila Hamilton: It may simply be a result of not paying enough attention to the failures. There’s very little tracking of the short- or long-term outcomes of people treated in most of America’s psychiatric centers. There’s very little accountability, or learning from the losses. One of the most shocking things I discovered in the aftermath of David’s suicide is that his psychiatrists and the in-patient care center where he was treated didn’t know he’d killed himself — they only learned of his death when I called the center days later. Imagine a heart surgeon who failed to follow up on a patient post-surgery!
JK: When you met David, he was juggling construction plans, a cappuccino and a pager. He ran his fingers through his hair. He fumbled with his wallet. You thought: “He drinks too much coffee.” Knowing what you do now, what would you think if you met a man who acted like that?
SH: I notice these behaviors in a different way now. When I meet people, I register the subtle signs of potential mental illness — extreme disorganization, or anxious mannerisms. I also note if the person is a creative type. Often the more creative personalities — writers, artists, filmmakers, musicians — experience one diagnosis or another. Even now, though, I couldn’t guarantee that I’d pick up on the signals that someone is struggling with an illness —detection is complicated and elusive when the person who is suffering denies the nature of his or her illness. I spoke to a psychiatric nurse recently who failed to piece together her husband’s major depression for nearly a decade. A primary care doctor wrote me to say he misses bipolar illness quite frequently, especially in his higher functioning patients.
JK: Psychiatrists spoke of David’s condition as ”recurrent manic episodes,” “mild depressions” and “anxiety disorder.” His explosive cursing, his infidelity and his lies were “the illness talking.” Were these second-rate psychiatrists or is bipolar that hard to diagnose?
SH: Bipolar disease is difficult to diagnose. Many primary care physicians miss it, especially bipolar II, because it presents as depression, combined with a high state of irritability and anxiety. The highly trained staff at the inpatient care centered argued over David’s diagnosis — some of the staff believed he suffered from complicated depression, others were convinced he had symptoms of Akathisia, a suicidal inducing condition sometimes brought on by anti-depressants. David’s case baffled them because he was resistant to medication.
JK: David tried to kill himself by cutting his wrists. And yet the hospital discharged him that night — he’d been treated and evaluated. How did that happen?
SH: In Oregon, a patient must be considered a risk to himself or others to be involuntarily committed. David convinced the intake staff that he was not a risk. It’s a common problem. He was persuasive, charismatic and insistent. Doctors can be persuaded by a patient’s belief in his or her own level of functioning.
JK: You write: “As my marriage crumbled, I felt more open and vulnerable than I had in years.” Explain.
SH: I did an awful lot of compartmentalizing and deflecting the nature of my marriage. I loved my daughter so fiercely, and I believed so steadfastly in the power of a daddy in his daughter’s life, that I put my fears aside and focused on how much he loved our daughter, even if he was hurting me. When I finally did a full accounting of how much companionship and love I’d missed, I knew I needed to change.
JK: The passage in which you tell your nine-year-old daughter her father is dead is tough to read. Tell me about the day you wrote that page.
SH: I was working on the story at our house, overlooking the west hills of Portland, and feeling completely stuck on the telling of the story. I pushed away from the desk to peer out our window and noticed the oak trees beginning to take on the gold and orange colors of fall. The similarity in the light and color from the previous fall triggered a cascade of memories that nearly floored me. I had convinced myself that I would need to leave that horrible day out of the story, but I couldn’t. It marked the moment Sophie and I had to decide — would we survive David’s choice? I wrote those pages knowing one day Sophie would read them. When she finally did, some seven years later, she said, “You got it completely right.” Her approval was so important to me.
JK: David broke into a lover’s house. After, a gun was missing. He was committed to a mental hospital. He assured his doctors he had no idea where the gun was — and they discharged him and he went off to kill himself. In a better world, that wouldn’t have happened. And, in a better world, you would be able to sue those doctors. Do you wish you could?
SH: No. Yes. No.m Would holding the people accountable who offered shoddy and substandard care bring David back? No. But would it help to usher in the kind of reforms that must take place in the mental health system? Yes. I’d be lying if I told you I hadn’t thought about holding the physician accountable for prescribing the meds that pushed David over into akathisia. Akathisia is a subjective, often misdiagnosed feeling of inner restlessness that can range from mild anxiety to a feeling of overwhelming doom, and it can be induced by antipsychotic medication, and in fact is highly correlated with suicide. But I also know that David’s friend and doctor was trying to help him. And I don’t want to discourage general physicians from helping others. I just want practitioners to be trained properly before administering potentially dangerous drugs. Ironically, the hospital where David received treatment has fired most of its psychiatric staff and had the rest apply for their jobs a second time. They are planning an emergency psychiatric center that will be based on a trauma-informed model of care, where the patient participates in his healing. People with lived experience will be asked not “What is wrong with you?” but “What happened to you?” This approach empowers the staff and the person suffering to cooperate. There will be somatosensory activities that are proven to help a traumatized brain heal-including yoga, mindfulness and music. The hospital will be a model for the nation. I couldn’t have hoped for a better outcome — and it’s happening without the lawyers.
JK: Knowing what you do now, what you would tell someone who might be bipolar? What would you tell his/her loved ones?
SH: I would tell that person that recovery is possible. I would also say that if he or she feels stuck in a relationship with a psychiatrist or psychologist who doesn’t believe in the tenets of recovery, they should find a new team of doctors, and would encourage the person to find a team that looks beyond the pharmaceutical approach to healing. For the last decade, the psychiatric profession has relied far too heavily on drugs, while most other industrialized nations are looking at a more holistic approach.
JK: Would you suggest a useful book on mental illness? A helpful web site?
SH: Bruce Perry’s The Boy Who Was Raised as a Dog is essential. It provides so much insight into the brain’s capacity to heal, and shows why trauma is the source of most of our major mental illness. On the Internet, go to www.FEMHC.org, the website of the Foundation for Excellence in Mental Health Care. FEMHC is comprised of the most passionate psychiatrists, psychologists, researchers, philanthropists, and people with lived experience. They are courageously changing the mental health system.
JK: Your daughter is now 18, and off to college. You’ve remarried. How often do you think about David? How often are you drawn back to those years of fear and confusion? Considering where you are now, does that nightmare feel like just that — a bad dream?
SH: I think about him every day. I have never had a single day of reprieve. I see David in Sophie’s bone structure, the curve of her ear, and the quickness and alertness of her mind. I miss his sense of humor; I miss the person he was and the person he could have become, if not for his illness. He missed out on so much beauty — especially in not being here to see our daughter turn into such a compassionate and wise adult.